Uterine Cancer

When cancer arises from the inner lining of the uterus (womb) it is known as endometrial cancer. When cancer arises from the muscular part of the uterus (womb) it’s known as uterine sarcoma. In women of reproductive age group, the endometrium thickens every month in preparation for a possible pregnancy. If the woman does not conceive, the endometrial lining is shed and the menstrual period occurs. After menopause due to hormonal imbalance the endometrial lining normally stops growing and shedding and thus menstrual periods stops. In women who have endometrial cancer, the uterine lining develops abnormal cells and have irregular bleeding.
Endometrial cancer is increasing all over the world. Endometrial cancer is usually seen in women over the age of 50 and thus after menopause, but up to 25% of cases may occur before the menopause. Obesity is a well-known risk factor for endometrial cancer at all age groups. Endometrial cancer are generally of two types they are divided based on the expression of hormone receptors and the tumor grade. The most common type is Type I which is hormone dependent and this is of the low grade type and commonly seen in obese women. Type II is of high grade type not hormone dependent and in this type women need be obese and Type II is associated with higher risk of metastasis and poorer outcome.
Where is uterus situated in the body?
The uterus is also known as the womb. It is a pear-shaped organ and is situated in the pelvis.
The uterus is divided into two parts: the upper bulky part is the body of the uterus and the lower narrow part is known as the cervix.
The thin inner layer of the uterus is called the endometrium. The thick outer layer is called the myometrium and is composed of muscle.
The body of the uterus can easily expand during pregnancy to hold a developing baby.
The junction of the uterus and the cervix is known as internal os (orifice) and the opening present at the lowermost part of the cervix is known as external os. The cervix connects the uterus to the vagina.
The main function of the uterus is to hold the baby during pregnancy and to regulate monthly menstrual cycles.


What are the causes?
Before we understand the causes, it’s important to understand the hormone that is responsible for causing endometrial cancer.
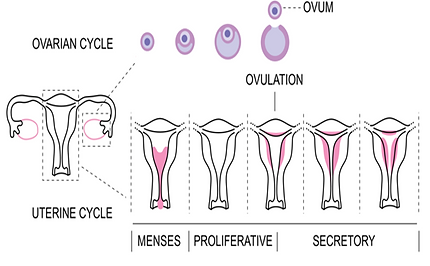
Normally, the menstrual cycle is divided into two phases:
-
In the first phase, the Follicular / Proliferative phase which happens immediately after menstruation is dependent on a hormone called oestradiol and this phase is for about two weeks, following which the ovulation happens (release of the egg from the ovary). After, ovulation happens another hormone is released called progesterone.
-
The second phase, the Luteal / Secretory phase, this phase starts after ovulation, and again this is for about two weeks. If conceptions don’t happen then the progesterone levels fall and menstruation occurs.
When a hormonal imbalance occurs such as excess of oestradiol the lining of the endometrium grows durationally and causes endometrial cancer.

Some of the risk factors for developing endometrial cancer:
Aging:
The risk of endometrial cancer has been seen to increase as women get older.

Genetic risk:
If you have inherited nonpolyposis colon cancer syndrome, also known as HNPCC or Lynch syndrome, your risk of developing colon and endometrial cancer is high. One in two women with this HNPPC syndrome will develop endometrial cancer at some point in their life. It is said to account for up to 5% of endometrial cancers.

Family history of endometrial cancer:
If you have a first-degree relative like mother,
sister, or daughter who had or have endometrial cancer this increases the risk of youhaving endometrial cancer.

Personal history of cancer:
If you have had experienced breast cancer or ovarian cancer
in the past then the risk of you developing endometrial cancer would be high.

On Tamoxifen:
If you have had a personal history of breast cancer and have been treated with tamoxifen(which is sometimes part of breast cancer treatment) remember that this tamoxifen can have an adverse effect on the endometrium and lead to endometrial cancer. Talk to your doctor if you are on tamoxifen and do not stop this medication with our proper medical advice.

Polycystic ovarian syndrome (PCOS):
If you have PCOS, you are at increased risk to develop endometrial cancer. In this condition since ovulation doesn’t take place you will have more oestradiol in your body and less of progesterone, thus excess of estrogen can lead to endometrial cancer.

Personal history of endometrial hyperplasia:
This is known as a precancerous condition for endometrial cancer. As the name suggests endometrial hyperplasia is a proliferation of cells of the endometrium. This hyperplasia can happen due to chronic exposure to estrogen with an insufficient amount of progesterone. For Eg: women taking estrogen tablets (as HRT treatment for menopause) or sometimes just a natural hormonal imbalance in women.

Overweight & obesity:
When you have high BMI (body mass index) due to being overweight or obese this increases the risk of endometrial cancer, that’s because fat gets converted into oestradiol hormone and more fat you have, you have more oestradiol in your body and thus you are at increased risk of developing endometrial cancer.

Metabolic syndrome
Women with metabolic syndrome are at increased risk of developing endometrial cancer. Metabolic syndrome includes obesity, diabetes, dyslipidemia, and hypertension.

No pregnancy (nullipara women):
Women who have never been pregnant are supposed to be at a higher risk of developing endometrial cancer.

The total number of menstrual cycles:
Early onset of menstruation and late menopause, that is having more menstrual cycles in a lifetime increases the risk of developing endometrial cancer, again for hormonal reasons.

What are the symptoms?
-
Vaginal bleeding apart from menstruation
-
Bleeding again after menopause
-
A watery discharge which is blood-tinged or brownish vaginal discharge
-
Bleeding in-between periods (intermenstrual bleeding)
-
Tummy pain / unexplained pelvic pain
-
Loss of appetite
-
Loss of weight
-
Feeling tired
-
Pain during urination
What tests will be required for diagnosis?
-
To confirm the diagnosis: The doctor will usually do a vaginal examination (internal examination) if you have symptoms that may possibly be like cancer.
-
Assessing the extent and spread:
-
First, you would be advised to have an ultrasound of the pelvis to check the thickness of the endometrium. The best way to perform this is through the transvaginal route (vaginal ultrasound). If the thickness of the endometrium is more then you would be advised to have an endometrial biopsy
-
Endometrial biopsy and histopathological examination: here a small tissue from the endometrium is taken to be examined in the laboratory. This is a minor procedure and can be done in an out-patient set-up without any anesthesia. In some cases where women are anxious, this can be done under sedation.
-
Further tests may be advised to assess if cancer has spread to other organs such as an ultrasound scan, a CT scan, PET CT an MRI scan, a chest X-ray, and blood tests.
-


Endometrial biopsy
What are the treatment options?
The main treatment for endometrial cancer is surgery. After the surgery you may need Radiotherapy and or chemotherapy and are called adjuvant therapies, meaning that they are used in addition to surgery.
Surgery :
-
Surgery is the first course of treatment for endometrial cancer. 90% of women with this cancer undergo some form of surgery. They are treated with hysterectomy (removal of womb and neck of the womb) and bilateral salpingo-oophorectomy (both fallopian tubes and ovaries) and lymph glands. Sentinel lymph node: This entails identifying and examining the nearest lymph glands the cancer is most likely to metastasise. If the cancer has not spread till here, it is likely that other glands are also cancer-free. So, in some cases, you may be advised to sentinel lymph node biopsy.
-
This surgery can be performed via an Open-abdomen procedure called laparotomy, this is the traditional surgical procedure.
-
Keyhole technique called laparoscopy or robotic surgery: these techniques associated with less pain, speedy recovery, small scars, and early discharge from the hospital.
-
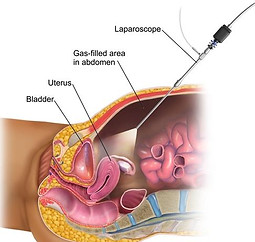
Laproscopy

Robotic Surgery

Open Surgery
In some cases radiation and or chemotherapy may be required, depending on your stage this is known as adjuvant treatment.
Radiation Therapy:
Radiation is a machine, which uses high-energy X-rays to kill cancer cells and stop their growth.
There are two ways of having radiation treatments:
-
Brachytherapy: Radiation is given through your vagina.
-
External beam radiation therapy: radiation is given from above your tummy.
Chemotherapy
-
In chemotherapy treatment drugs are used to kill or slow the growth of cancerous cells. It’s usually given through an IV injection.
-
You will be told that you need chemo with radiation; this type of treatment is called chemoradiation.
-
Adding chemo during radiation makes the radiation to be more effective. You might also get only chemotherapy treatment if your cancer has spread to other organs.


Follow-up after treatment:
-
You should strictly go for follow-up with your doctor as per their advice.
-
In addition to receiving treatment for uterine cancer your success of treatment will depend only when you have regular follow-up.
